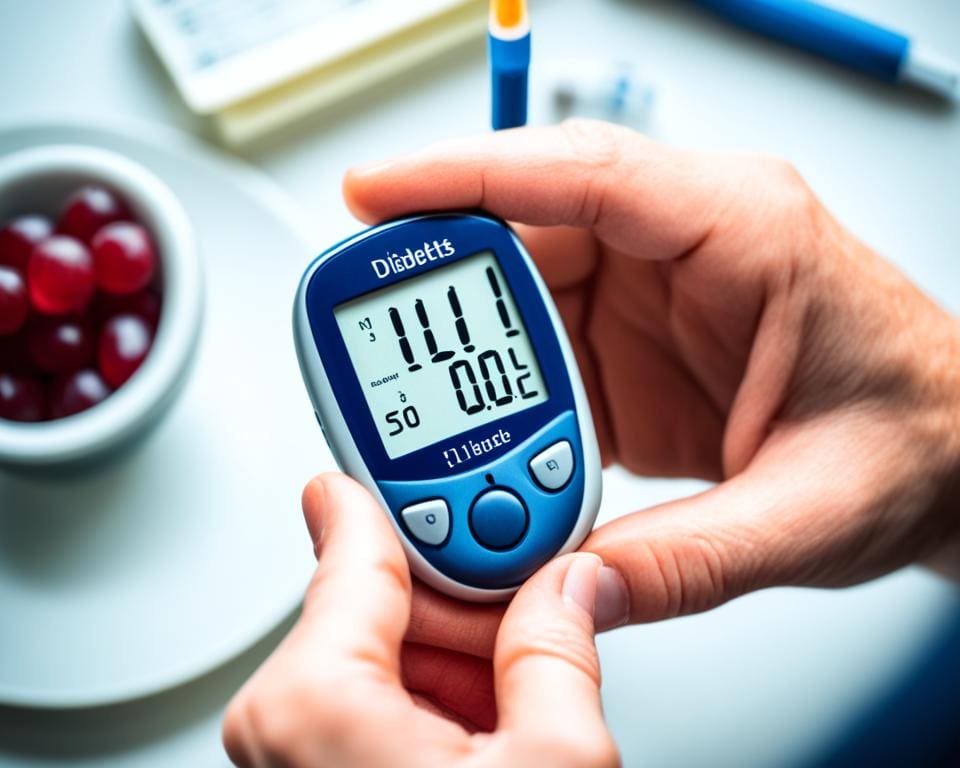
Drinking enough water is key for everyone, but it’s even more important if you have diabetes. The Centers for Disease Control & Prevention say 1 in 10 Americans have diabetes1. Water is crucial for managing diabetes and keeping blood sugar levels healthy. It helps get rid of extra glucose, prevents dehydration, and boosts overall health1.
Medicine, exercise, and a healthy diet are important for diabetes, but don’t forget about water. Drinking enough helps control blood sugar by moving glucose and insulin around your body1. If you have diabetes, you lose water faster, so you might need more to stay hydrated2. Drinking more water can help when your blood sugar is high to avoid dehydration1.
The Institute of Medicine suggests drinking about 13 cups of water a day for men and 9 cups for women1. Your water needs can change based on your age, how active you are, your weight, and the weather1. Keeping track of how much water you drink and slowly increasing it can help you stay hydrated and manage your blood sugar better1.
Lifestyle changes, like drinking enough water, are key to managing blood sugar and avoiding diabetes problems1. By drinking water, you’re taking a big step towards better diabetes care and health.
Key Takeaways
- Staying hydrated is crucial for managing diabetes and maintaining healthy blood sugar levels.
- Water helps flush out excess glucose, prevents dehydration, and supports overall health.
- People with diabetes have a higher risk of dehydration due to increased water loss.
- Recommended water intake varies based on factors like age, activity level, and weather.
- Proper hydration, along with medication, exercise, and a healthy diet, is essential for diabetes management.
The Connection Between Diabetes and Dehydration
People with diabetes often face a higher risk of dehydration, especially when it’s hot3. This happens because high blood sugar makes the body lose fluids through more frequent urination3. If not managed, this can lead to dehydration.
How High Blood Sugar Affects Fluid Levels
High blood sugar can make it hard for the body to stay hydrated, which is a big risk for those with diabetes4. The kidneys work harder to get rid of the extra sugar, causing thirst and dry mouth4. Drinking enough water is key for keeping blood sugar stable in people with type 2 diabetes5.
A study showed that not drinking enough water can affect how well blood sugar responds5. Drinking about 100 ounces a day helped people with type 2 diabetes control their glucose levels better5.
Diabetes and Increased Urination
Diabetes often leads to more trips to the bathroom as the body tries to get rid of sugar through urine3. This can cause a lot of fluid loss, so it’s important for diabetics to drink enough water to stay hydrated3. Not drinking enough water can make it harder for the body to manage insulin over time5.
A study followed healthy adults for nine years and found that drinking less than half a liter of water daily raised the risk of high blood sugar5.
Keeping blood sugar stable and staying healthy is crucial for diabetics. They should drink plenty of water to avoid dehydration3. Experts suggest drinking 91 ounces a day for women and 125 ounces for men, with some from fruits and veggies5.
| Condition | Recommended Daily Water Intake |
|---|---|
| Women | 91 ounces |
| Men | 125 ounces |
Drinking enough water helps diabetics keep their blood sugar stable, manage insulin, and lower dehydration risks. In hot weather, it also helps control blood sugar and insulin levels5.
Diabetes Thirst: A Symptom of Mild Dehydration

Feeling very thirsty is common in diabetes. It happens in diabetes mellitus and diabetes insipidus6. High blood sugar and peeing a lot can make you very thirsty6. This dehydration is a big reason for the thirst and peeing a lot in people with diabetes7.
When your body loses water because of high blood sugar, it gets thirsty to drink more. But even after drinking a lot, you might still feel thirsty. This is because your kidneys keep making more urine to get rid of the extra sugar. This thirst is a key sign of diabetes, along with peeing a lot, feeling very tired, blurry vision, and losing weight without trying7.
Prolonged dehydration can cause nausea, dizziness, headaches, fainting, and higher blood sugar levels in people with diabetes6.
To manage diabetes thirst and lower your a1c, try these tips:
- Drink water all day to stay hydrated
- Suck on sugar-free hard candy or chew sugar-free gum to help make saliva6
- Reduce caffeine to avoid dehydration
- Use a humidifier to add moisture to the air, especially in dry places6
- Try over-the-counter saliva substitutes to ease dry mouth6
| Diabetes Symptom | Cause | Management Strategy |
|---|---|---|
| Excessive thirst (polydipsia) | High blood sugar and frequent urination | Stay hydrated, limit caffeine, use a humidifier |
| Frequent urination (polyuria) | Body trying to flush out excess glucose | Manage blood sugar levels through diet, exercise, and medication |
| Fatigue | Disruption in the body’s energy usage due to high blood sugar | Maintain stable blood sugar levels, get adequate sleep |
If you keep feeling thirsty, peeing a lot, tired, seeing blurry, or losing weight without trying, see a doctor fast7. Taking care of diabetes with medicine, changing your lifestyle, and checking your levels often can lower your risk of problems from high blood sugar67.
Diabetic Ketoacidosis: A Severe Complication of Dehydration
Diabetic ketoacidosis (DKA) is a serious condition that can happen when someone with diabetes has high blood sugar for a long time. It’s more common in people with type 1 diabetes and can cause severe dehydration if not treated quickly89. The chance of getting DKA varies widely, from 0 to 56 cases per 1000 people each year. Women and non-Whites are more likely to get it10.

What is Diabetic Ketoacidosis?
DKA happens when the body can’t use insulin properly. This makes it start burning fat for energy instead, creating ketones. These ketones make the blood too acidic, causing ketoacidosis8. DKA is marked by very high blood sugar, ketones in the urine, and a condition called ketoacidosis8.
DKA also causes dehydration because of sugar in the urine and other factors. This dehydration can lead to serious problems with electrolytes, like losing a lot of potassium, sodium, and chloride8. It can also harm the kidneys, causing more electrolyte imbalances8.
Symptoms of Diabetic Ketoacidosis
DKA can start fast, often in just 24 hours. Its symptoms include:
- Dry skin and flushed face
- Headaches and muscle stiffness
- Nausea and vomiting
- Abdominal pain
- Rapid, shallow breathing (Kussmaul respirations)
- Fruity-scented breath
- Confusion and drowsiness
In bad cases, DKA can make someone lose consciousness and even lead to a coma8. Sadly, 1% to 8% of people with DKA might not survive9. People over 65, those under 5, and those with a family history of diabetes or autoimmune diseases are more likely to get DKA9.
People with diabetes, especially type 1, need to know the risks and signs of DKA. Risk factors include missing insulin, being newly diagnosed, and certain health issues9. If you have symptoms of DKA or your blood sugar is over 300 mg/dL, get help right away to avoid serious problems9.
The Importance of Hydration in Managing Diabetes
Staying hydrated is key for managing diabetes and keeping you healthy. If you have diabetes, your body can’t regulate blood sugar well. Drinking enough water helps get rid of extra glucose through urination, which keeps your blood sugar levels in check11.
For people with diabetes, staying hydrated is crucial because not drinking enough water can raise your blood sugar levels11. The Institute of Medicine suggests drinking about 13 cups of water a day for men and 9 cups for women1. But, your needs can change based on your age, how active you are, your weight, and the weather1.
Drinking Water Helps Flush Out Excess Glucose
When you eat carbs, your body turns them into glucose, which goes into your bloodstream. Insulin, made by the pancreas, helps your cells use this glucose for energy. But if you have diabetes, you might not have enough insulin or your body can’t use it right, leading to high blood sugar.
Drinking water helps your body get rid of extra glucose by making you urinate more. This is especially important for diabetes patients, as high blood sugar can make you urinate a lot, leading to dehydration. By drinking enough water, you help your body control blood sugar levels and avoid diabetes complications.
Adequate hydration is essential for maintaining healthy blood sugar levels and overall well-being when managing diabetes.
Staying Hydrated Supports Overall Health
Being hydrated is also key for your overall health. Water is a big part of your body, making up 50% to 70% of your weight11. It’s important for many bodily functions, like:
- Regulating body temperature
- Transporting nutrients and oxygen to cells
- Removing waste products
- Lubricating joints
- Supporting skin health
People with diabetes are more likely to have heart problems. Drinking enough water helps keep your blood volume and circulation healthy, which is easier on your heart. Staying hydrated also keeps your kidneys working right, prevents dehydration issues, and helps your heart health.
To make sure you’re drinking enough fluids, try to drink water all day. Keep a water bottle with you and set reminders to drink. Watching the color of your urine can also tell you if you’re hydrated. Healthy urine is light yellow or almost clear, while dark urine means you need more water1.
| Hydration Tips for People with Diabetes |
|---|
| 1. Carry a refillable water bottle and drink from it regularly |
| 2. Set reminders or alarms to prompt you to drink water |
| 3. Flavor water with slices of lemon, lime, or cucumber for variety |
| 4. Choose water-rich foods like fruits and vegetables |
| 5. Monitor urine color to assess hydration status |
Recommended Water Intake for People with Diabetes

For people with diabetes, drinking enough water is key. Men should aim for about 125 ounces (15.5 cups or 3.7 liters) of water daily11. Women should try to drink around 91 ounces (11.5 cups or 2.7 liters)11. The European Food Safety Authority suggests women drink 1.6 liters (about eight 200ml glasses) and men 2 liters (around ten 200ml glasses) a day12.
Your water needs can change based on your age, how active you are, your weight, and the weather. Even if you have well-controlled diabetes, you might not need more water than others. But, if your blood sugar is high, drinking more water is crucial. It helps prevent dehydration and keeps blood sugar in check. Water makes up a big part of your body, between 50% to 70%11. Your body also needs a balance of water and glucose in your blood11.
A 2011 study found that drinking more than one liter of water daily could lower the risk of high blood sugar by 28%. Those who drank more water might prevent or delay diabetes12.
Drinking water helps control blood sugar by letting more glucose leave your blood without raising your sugar levels12. This is very important for people with diabetes. Dehydration is a risk, and drinking more water helps your body when it’s getting rid of extra glucose through urine12.
To figure out how much water you need, talk to your healthcare provider. They can look at your diabetes plan, medicines, and health to give you advice. This advice will help you manage your diabetes diet and keep your blood sugar in check.
| Gender | Recommended Daily Water Intake |
|---|---|
| Men | 125 ounces (15.5 cups or 3.7 liters)11 |
| Women | 91 ounces (11.5 cups or 2.7 liters)11 |
Other Beverages to Help Stay Hydrated

Water is the top choice for staying hydrated, but there are other diabetes-friendly drinks that can help too. Adults need at least 64 ounces of water a day for good hydration. Men need about 100 ounces, and women 75 ounces13. If plain water is hard to drink, there are ways to make it tastier without hurting your blood sugar levels.
Flavoring Water with Lemon or Lime
Adding fresh lime or lemon juice to your water can make it taste better. This trick makes drinking water fun, even if you don’t like plain water. Plus, lemon and lime give you vitamin C, which is good for your health.
Herbal Teas, Skim Milk, and Sugar-Free Coffee
Herbal teas without caffeine are great for staying hydrated with diabetes. There are many flavors to choose from, so you can find one you like. Skim milk is also good, offering calcium and protein without the fat and carbs in whole milk. A glass of skim milk has about 12 grams of carbs, less than the 16 grams in chocolate milk14.
If you like coffee, go for sugar-free options to keep your blood sugar stable. A chai latte from a coffee shop has 33 grams of carbs. Coffeehouse mochas can have over 300 calories and 40 grams of carbs14. Sugar-free drinks let you enjoy your favorites without the risks.
“As of October 2022, approximately 34.2 million people are living with diabetes in the United States, and another 88 million have prediabetes13. Making informed choices about the beverages you consume can play a significant role in managing your condition and maintaining overall health.”
These diabetes-friendly drinks can help you stay hydrated, but drink them in moderation. Always check your blood sugar levels. By choosing wisely and staying hydrated, you can manage your diabetes better and feel great.
Drinks to Avoid When Managing Diabetes
When dealing with diabetes nutrition, watch what you drink closely. Some drinks can make your blood sugar spikes quickly. Here are some drinks you should limit or avoid to manage your diabetes better.

Energy Drinks, Fruit Juices, and Sodas
Energy drinks, fruit juices, and sodas are often loaded with sugar. A single 12 oz can of soda has about 38.5 g of carbs15. Energy drinks like Red Bull have over 26 g of sugar and 75 mg of caffeine in an 8.4 oz serving15. Drinking these can up your risk of getting prediabetes by 46% if you have more than three a week15.
The Risks of High-Sugar Beverages
Drinks with lots of sugar don’t just raise your blood sugar. They also add extra calories. Drinking two sugar-sweetened drinks a week can up your risk of type 2 diabetes15. Even drinks with artificial sweeteners might raise your risk of type 2 diabetes and heart disease, but we need more studies15.
| Beverage | Carbohydrate Content per Serving |
|---|---|
| Soda (12 oz) | 38.5 g |
| Energy Drink (8.4 oz) | 26 g |
| Tomato Juice (8 oz) | 10 g |
| Sports Drink (8 oz) | 19 g |
Instead of sugary drinks, try water, unsweetened tea, or coffee. Coffee and tea, especially green tea, might lower your risk of type 2 diabetes15. For flavor, add fresh fruits like lemon or lime to your water for a tasty, low-carb drink.
Remember, when it comes to alcohol, drink in moderation. The American Diabetes Association says that’s up to one drink a day for women and two for men15.
Choosing wisely about what you drink can help you manage your blood sugar and lower the risk of blood sugar spikes. Talk to your doctor or a dietitian to make a meal plan that fits your needs and likes.
Recognizing the Symptoms of Dehydration
Dehydration is a big concern for people with diabetes. It can cause high blood sugar and other health problems. Knowing the signs of dehydration helps you act fast to prevent it from getting worse. Mild dehydration in kids means losing 3%-5% of their body weight16.
Mild Dehydration Symptoms
Mild dehydration shows up as:
- Thirst
- Dry mouth and lips
- Fatigue
- Headache
- Dizziness
- Dark-colored urine
These signs are easy to miss but are key warnings your body needs more fluids. Diabetes patients might pee a lot, which can lead to dehydration16. Drinking enough water is key for health, especially when you’re sick, pregnant, or active16.
Severe Dehydration Symptoms
Not treating dehydration can make it worse, even dangerous. In kids, severe dehydration means losing over 10% of their body weight16. Signs of severe dehydration are:
- Extreme thirst
- Dry skin that doesn’t bounce back when pinched
- Rapid heartbeat
- Rapid breathing
- Sunken eyes
- Confusion or irritability
- Fainting
Severe dehydration is an emergency. It can cause serious problems like heat exhaustion, seizures, and even death16.
| Mild Dehydration Symptoms | Severe Dehydration Symptoms |
|---|---|
| Thirst | Extreme thirst |
| Dry mouth and lips | Dry skin that doesn’t bounce back when pinched |
| Fatigue | Rapid heartbeat |
| Headache | Rapid breathing |
| Dizziness | Sunken eyes |
| Dark-colored urine | Confusion or irritability |
| Fainting |
People with diabetes should watch their hydration closely. Spotting dehydration early helps you rehydrate and avoid serious issues.
Factors That Can Worsen Dehydration
Many things can make dehydration worse for people with diabetes. This makes managing diabetes well key. People who work or exercise outside in the heat are more likely to get dehydrated and sick17. Anyone can get dehydrated if they don’t drink enough water when it’s hot or if they exercise a lot17.
Other things that can make dehydration worse include hard exercise, not drinking enough water, and drinking alcohol18. Drinking alcohol can make you pee more and lose fluids18. While caffeine itself doesn’t dehydrate you, too much coffee with sugar can raise your blood sugar18.
Things like throwing up or diarrhea, hard exercise, extreme heat or cold, and being sick make you need more fluids to stay hydrated17.
Drinking enough water is key to keeping your blood sugar stable and avoiding dehydration problems. To prevent dehydration, you should:
- Eat right
- Keep a healthy weight
- Exercise regularly
- Check your blood sugar often
- Eat balanced meals
- Avoid sugary drinks
- Drink less alcohol
- Control how much you eat19
| Dehydration Risk Factors | Prevention Strategies |
|---|---|
| Hot and humid weather | Drink more water |
| Strenuous exercise | Drink water before, during, and after working out |
| Alcohol consumption | Drink less and switch to water |
| High-sugar beverages | Choose water or drinks without sugar |
Knowing what can make dehydration worse and how to prevent it helps people with diabetes manage their condition better. This can lower the risk of dehydration problems.
When to Consult a Doctor About Dehydration
Keeping hydrated is key for those with diabetes to avoid complications. If you feel thirsty, have a dry mouth, or your urine looks dark, drink more fluids. Also, focus on diabetes care through meds and lifestyle changes to balance your fluids. Signs of dehydration include thirst, dry mouth, dizziness, headaches, dark urine, and less urine20.
If you can’t control your blood sugar, talk to your doctor about your diabetes meds. They can check what you need and suggest the best treatment to keep you hydrated and manage your diabetes.
Adjusting Diabetes Medication
Your doctor might change your diabetes meds if your hydration or blood sugar levels change. This is key if you often get dehydrated or if your blood sugar stays high. Adjusting your meds can help balance your diabetes and prevent dehydration.
Severe Dehydration and Diabetic Ketoacidosis
Severe dehydration shows as confusion, low blood pressure, fast breathing and heart rate, and fever. You should get medical help right away20. This kind of dehydration is serious and needs quick treatment, like fluids through a vein20.
If you have diabetic ketoacidosis (DKA) signs like nausea, vomiting, sweet breath, shortness of breath, or confusion, it’s an emergency. DKA is a serious diabetes issue that happens when your body makes too many blood acids. Without treatment, it can cause seizures, brain damage, or even death21. Getting medical help fast is key to avoiding these bad outcomes and keeping your diabetes under control.
“Dehydration can be a serious complication of diabetes, but with proper diabetes care and attention to hydration, you can maintain your health and well-being.”
The Role of Water in Lowering Blood Sugar
Water doesn’t directly lower blood sugar, but it’s key for managing diabetes and blood glucose. The Centers for Disease Control and Prevention say 13% of Americans and 25% of those over 65 have diabetes22. Drinking water helps clear out extra glucose by making you urinate more. This is good for people with diabetes when their blood sugar is too high.
A 2021 review looked at studies and found that drinking more water can lower the risk of high blood sugar23. Water has no carbs or calories, making it a great choice for people with diabetes. It won’t raise their blood sugar levels.
Staying hydrated is just part of the story. Eating right and living healthily also helps control diabetes and blood glucose. Women should aim for about 25 grams of fiber a day, and men should aim for 35 grams23. Foods high in fiber can slow down how fast glucose gets into your blood, helping to keep blood sugar levels stable.
Adults need 7 to 8 hours of good sleep each night to keep blood sugar levels and insulin sensitivity in check23.
Not sleeping well can make you hungrier and gain weight, which can mess with your blood sugar22. High blood sugar can also mean you’re not getting enough chromium and magnesium, which help control blood sugar22. Foods like beef, chicken, turkey, and whole grains are good sources of chromium23. Eating a lot of magnesium can lower your risk of diabetes. Foods high in magnesium include dark leafy greens, squash, and pumpkin seeds, as well as tuna, whole grains, and bananas23.
Adding water, a balanced diet, and healthy habits to your day can really help with diabetes control and managing blood glucose.
Hydration Tips for People with Diabetes
Keeping up with hydration is key for managing diabetes and living a healthy life. Here are some tips to help you stay hydrated every day.
Drinking Water Throughout the Day
Drinking water regularly is a great way to stay hydrated. Carry a refillable water bottle with you to remind you to drink often. Women should aim for about six and a half cups of water a day, and men should go for eight and a half cups24. Drinking water helps keep your blood sugar stable and supports your health.
Avoiding Excessive Fluid Intake at Night
It’s important to not drink too much fluid before bedtime. Too much liquid can make you get up and go to the bathroom a lot at night, which can disrupt your sleep. This is called nocturia. Listen to your body and find a balance to stay hydrated without affecting your sleep.
FAQ
Why is drinking water important for managing diabetes?
Drinking water is key for managing diabetes. It helps clear out extra glucose through urination. This prevents dehydration and supports overall health. Staying hydrated helps keep blood sugar levels in check and supports bodily functions.
How does high blood sugar affect fluid levels in the body?
High blood sugar makes the kidneys work harder to remove glucose. This leads to more urination and fluid loss. If not replaced, dehydration can happen. It’s vital to drink enough water to manage diabetes.
Is excessive thirst a symptom of diabetes?
Yes, feeling very thirsty is an early sign of diabetes. It’s a sign of mild dehydration. This happens when the body loses too much water due to high blood sugar levels.
What is diabetic ketoacidosis, and how is it related to dehydration?
Diabetic ketoacidosis (DKA) is a serious diabetes complication. It happens when the body uses fat for energy instead of sugar. This leads to a buildup of ketones in the blood, causing severe dehydration and fluid loss.
How much water should people with diabetes drink daily?
The Institute of Medicine suggests 13 cups of water a day for men and 9 cups for women. But, needs can change based on age, activity, weight, and weather. It’s best to talk to a healthcare provider to find out how much water you need with diabetes.
What other beverages can help people with diabetes stay hydrated?
Besides water, drinks like lemon or lime water, caffeine-free herbal teas, skim milk, and sugar-free coffee can help. These options add variety and make staying hydrated more fun.
What drinks should people with diabetes avoid?
Avoid drinks that cause quick rises in blood sugar. This includes energy drinks, fruit juices, and sodas because they’re high in sugar. These drinks can raise blood glucose and add extra calories.
What are the symptoms of dehydration in people with diabetes?
Mild dehydration can cause dry mouth, thirst, headaches, dry eyes, and dry skin. Dark-colored urine, dizziness, and feeling tired are also signs. Severe dehydration can lead to low blood pressure, a weak pulse, and confusion.
Can drinking water help lower blood sugar levels?
Drinking water doesn’t directly lower blood sugar. But, it’s important for managing diabetes by not raising blood glucose. It helps clear out excess glucose through urination, which is good for high blood sugar levels.
What are some tips for staying hydrated when managing diabetes?
To stay hydrated, drink water regularly throughout the day. Using a refillable water bottle can help. But, don’t drink too much before bed to avoid waking up to go to the bathroom a lot.
Source Links
- https://www.eatingwell.com/article/8061842/how-much-water-do-you-need-when-you-have-diabetes/
- https://www.cdc.gov/diabetes/articles/managing-diabetes-in-the-heat.html
- https://www.abbott.com/corpnewsroom/diabetes-care/staying-hydrated-with-diabetes–a-balancing-act.html
- https://www.diabetes.co.uk/dehydration-and-diabetes.html
- https://www.everydayhealth.com/type-2-diabetes/symptoms/can-chronic-dehydration-lead-type-2-diabetes/
- https://www.webmd.com/diabetes/diabetic-thirst
- https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-symptoms/art-20044248
- https://emedicine.medscape.com/article/118361-overview
- https://www.webmd.com/diabetes/ketoacidosis
- https://www.ncbi.nlm.nih.gov/books/NBK560723/
- https://blog.walgreens.com/health/diabetes/to-manage-your-diabetes-staying-hydrated-is-key.html
- https://www.diabetes.co.uk/food/water-and-diabetes.html
- https://www.eatingwell.com/article/8009374/best-and-worst-hydration-drinks-for-people-with-diabetes/
- https://www.webmd.com/diabetes/ss/slideshow-diabetes-friendly-drinks
- https://www.everydayhealth.com/type-2-diabetes/best-and-worst-drinks-for-type-2-diabetes/
- https://www.webmd.com/a-to-z-guides/dehydration-adults
- https://www.mayoclinic.org/diseases-conditions/dehydration/symptoms-causes/syc-20354086
- https://www.verywellhealth.com/diabetes-and-dehydration-6501265
- https://www.medicalnewstoday.com/articles/can-dehydration-cause-high-blood-sugar
- https://www.healthdirect.gov.au/dehydration
- https://www.nhsinform.scot/illnesses-and-conditions/nutritional/dehydration/
- https://www.gradyhealth.org/blog/8-ways-to-lower-your-blood-sugar/
- https://www.healthline.com/nutrition/14-ways-to-lower-blood-sugar
- https://health.umms.org/2023/02/15/staying-hydrated-when-you-have-diabetes/